How Chronic Wounds Occur in Diabetes Patients?
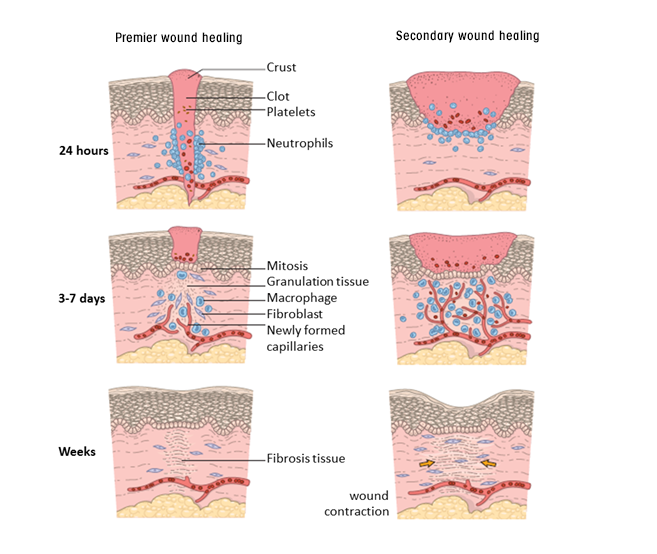
Due to the insufficient nutrition of the tissue, the treatment becomes more difficult as a result of infection in the area that does not heal.
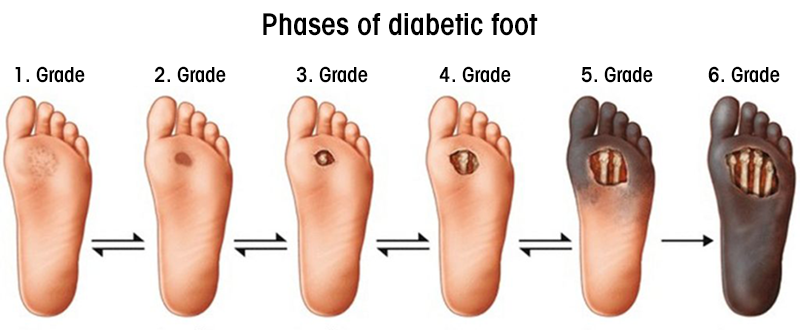
In diabetic patients, the problem of healing wounds arises as a result of the weakening of the defense system and deterioration of the nerves (neuropathy), especially in the legs, and blockage of the vessels.
In diabetic patients, even the wound that starts with a small rash is very important, it is the starting signal of a large chronic wound and requires careful follow-up and treatment. Outpatient chronic wounds occur in most patients with this condition. If adequate treatment is not done in patients with chronic wounds, poor results leading to amputation and ultimately death are seen.
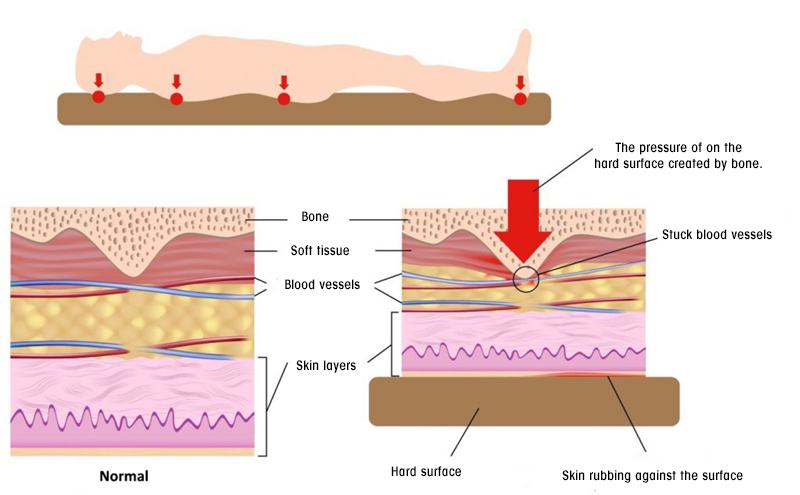
Pressure and Bed Sores
Bed sores, more commonly defined as "pressure ulcers", begin with the deterioration of blood supply in parts of the body that are exposed to high pressure and result in scar formation. It is not possible to heal the wound unless the pressure is removed and blood supply is regulated.
Although it often occurs in bedridden patients, these wounds can develop in any area with prolonged pressure, for example on the sitting bones in wheelchair-bound people.
Burn Wounds
As medical, burn is the loss of vitality of the skin with high heat. Depending on the height of the heat or the duration of contact, the superficial, middle and deep layers of the skin can burn and become dead. Burns can be comprised because of by contact with hot water or steam, contact with hot solid materials, contact with acid or alkaline chemicals, electric current or radiation.
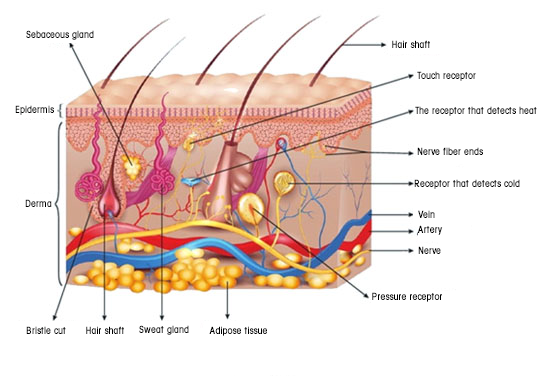
First degree burns (epidermal burn) are superficial. They affect the top layer of the skin called the epidermis. Edema may occur and there is no blisters, which we usually call bulla on the skin. The wound is red, dry and painful. It heals in a short time without leaving a scar. Sunburns fall into this class.
Second-degree burns also affect part of the dermis, the deep layer of the skin. It is mostly occured because of hot water, contacting with flame or hot object. Tissue damage is more than 1st degree burns, they are very painful, inflammatory burns. It heals in 2-3 weeks with dressings. Sometimes it may be necessary to resort to surgical treatment methods.
Third-degree burns are those that affect the entire (all layers) of the skin. The sensation of pain in the skin has disappeared and the color of the burnt area has changed from pink-red to brown and whitish, yellowish. They do not heal spontaneously. There is a high probability of infection and edema. They require surgical intervention and good care, take a very long time to heal and leave a scar.
How Should Burn Treatment Be?
In first degree burns, there is damage to the top layer of the skin. Sunburns are this kind of burns. Cooling the skin, topical anesthetic drugs, moisturizing and oily creams can be used in treatment. The skin in the burned area is shed superficially within 1-2 weeks.
In second degree burns, the upper layer of the skin is completely burned. Healing occurs with the proliferation of cells from the sebaceous glands, sweat glands and hair follicles in the subcutaneous layer. Second degree burns are divided into two subclasses, superficial and deep, according to the amount of loss in the healing skin appendages. There is no scar in a superficial 2nd degree burn, but a deep 2nd degree burn heals by leaving a scar. Blisters in the burned area should be protected. It is followed up with appropriate dressings. The recovery period is between 1 week and 10 days in superficial burns. In deep second degree burns, recovery is between 2-3 weeks.
In third degree burns, there are no skin patches left to renew the skin. Healing occurs with the skin that develops from the burned edges and a disturbing scar develops. Skin transplantation can be applied to the burn area to prevent poor wound healing. While small areas heal by leaving scars with dressings, large areas take a long time to heal, and if infection develops during this time, life-threatening may occur. Burns in the joint and neck area may cause restriction of joint and neck movements. Skin transplantation accelerates healing and prevents the development of loss of function. Scars develop less in skin transplanted areas. Treatment of 2nd degree and 3rd degree burns should be done by a burn specialist and should be followed with closed dressings.